Children
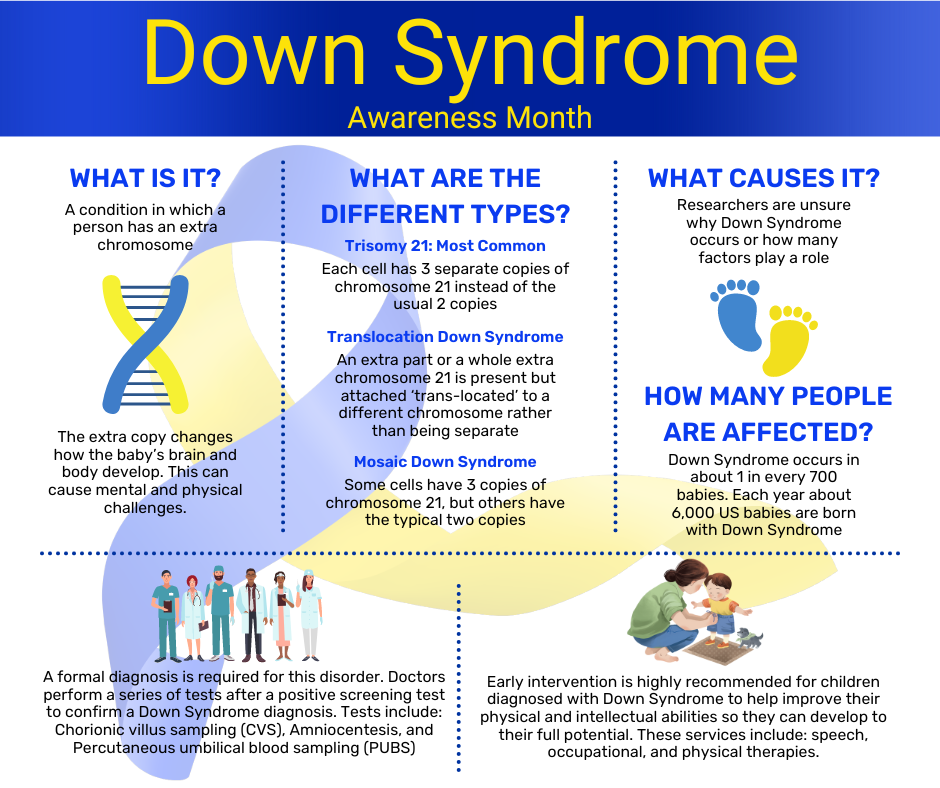
Down Syndrome Awareness Month
October 16, 2023This month we have the opportunity to raise public awareness about the condition Down Syndrome, as we advocate for the inclusion and acceptance of people with Down Syndrome. It is an unfortunate fact that people with Down Syndrome continue to face stereotypes and misconceptions about their abilities. We urge you to take this month to learn more about this condition and help us to spread the message of acceptance and respect for all people with Down Syndrome all year round.
What is Down Syndrome?
Down Syndrome is a genetic condition that occurs when a person is born with an extra chromosome. People are typically born with 46 chromosomes, but a person with Down Syndrome has an extra copy or part of an extra copy or chromosome 21.
There are three different types of Down Syndrome, and they are all dependent on how the extra chromosome 21 presents within the diagnosed person.
The most common type of Down Syndrome is called Trisomy 21, and about 95% of people who are diagnosed with Down Syndrome are diagnosed with this type. Trisomy 21 means that each cell within the body has three copies of chromosome 21 instead of the usual two copies.
The second most common type of Down Syndrome is called Translocation Down Syndrome and only about 3% of people diagnosed with Down Syndrome have this type. Translocation Down Syndrome occurs when an extra part or a whole extra chromosome 21 is present but attached ‘trans-located’ to a different chromosome, rather than being separate as is the case of Trisomy 21.
The least common type of Down Syndrome is called Mosaic Down Syndrome and only 2% of people who are diagnosed with Down Syndrome have this type. Mosaic Down Syndrome means that some of the cells in the body have three copies of chromosome 21, but other cells in the body still only have the typical two copies. Because only some of the cells in the body contain this additional chromosome this type of Down Syndrome presents less dominantly in physical features than the other two.
How do I know if my child has Down Syndrome?
About 6,000 babies are born with Down Syndrome in the US every year: that’s about 1 in every 700 babies. Down Syndrome can be detected in utero with screening tests and/or diagnostic tests. Screening tests can tell you if your pregnancy has a higher or lower chance of resulting in a baby with Down Syndrome, but they do not provide an absolute diagnosis. Diagnostic tests on the other hand, can typically detect whether a baby will have Down Syndrome. Diagnostic tests can be risky and are not generally performed until after a positive screening test. They include Chorionic villus sampling (CVS) which examines the material from the placenta, Amniocentesis which examines the amniotic fluid, and Percutaneous umbilical blood sampling (PUBS) which examines the blood from the umbilical cord. Each of these tests look for changes in the chromosomes that would indicate a Down Syndrome diagnosis.
What causes Down Syndrome?
Researchers know that Down Syndrome occurs when a person is born with an extra chromosome 21, but they are unsure how or why the extra chromosome forms. Many researchers believe that there are several different factors that play a role in whether the extra chromosome 21 will form in utero, but they are not entirely sure what those factors are. It is known that the likelihood of a baby being born with Down Syndrome increases with a mother’s age, but because more women give birth before they turn 35, more babies with Down Syndrome are born to women under 35 years of age. Nothing that a parent does during pregnancy is known to cause Down Syndrome.
What are the complications of Down Syndrome?
About half of people with Down Syndrome also have a congenital heart defect. They are also more prone to hearing loss, ear infections, obstructive sleep apnea, respiratory issues, eye diseases, poor eyesight, Alzhemer’s disease, leukemia, thyroid disorders and intestinal blockages at birth that require surgery.
In addition to the physical complications that can come along with Down Syndrome, it can also cause intellectual and developmental symptoms that can lead to cognitive impairment. Similar to the physical complications these symptoms can range from mild to moderate and include short attention span, poor judgement, impulsive behavior, slow learning, and delayed language and speech development.
What is the treatment for Down Syndrome?
Making sure that a child with Down Syndrome receives services early in life will help them to improve their physical and intellectual abilities and ensure that they reach their full potential into adulthood. Most of the services recommended for children with Down Syndrome focus specifically on helping them minimize the effects of any intellectual or developmental symptoms the condition is responsible for. Early intervention services include speech therapy, occupational therapy, and physical therapy.
These therapies can be beneficial to children with Down Syndrome past the years of early intervention as well. Each person with Down Syndrome has different talents, and they all have the ability to thrive. Down Syndrome is a lifelong condition and children with Down Syndrome may need extra help or attention in school, but with the proper treatment plan and early intervention many people with Down Syndrome are able to be mainstreamed and attend regular classes with their peers.
If you child has been diagnosed with Down Syndrome and you are interested in learning more about how Schreiber’s Pediatric Therapies can help your child visit: http://www.schreiberpediatric.org/therapy-services/
As a nationally recognized pediatric facility, the Schreiber Center for Pediatric Development provides family-centered education and therapy programs for infants, children and adolescents with disabilities, developmental delays, and acquired injuries. Our goal-oriented approach maximizes each child’s ability to function independently within the community.
20 Tips for a Sensory Processing Disorder Friendly Halloween
October 12, 2023Halloween, with its costumes, candies, and eerie decorations, is a thrilling time for many children. However, for those with Sensory Processing Disorder (SPD), this holiday can present unique challenges. SPD can make the sensory overload of Halloween overwhelming. But fear not! In this blog post, we’ll share some invaluable sensory Halloween tips and ideas to ensure your child has a comfortable and enjoyable Halloween experience.
1. Prepare Your Child:
Start by preparing your child for Halloween. Explain the concept of the holiday and what to expect. Videos can be a great tool to help them visualize what Halloween is all about.
2. Visual Calendar:
Create a visual calendar to help your child countdown to Halloween. Seeing the days pass can provide a sense of predictability and reduce anxiety.
3. Pumpkin Alternatives:
Many children with SPD don’t enjoy carving pumpkins. Encourage them to paint or draw on them instead.

4. Comfortable Costumes:
Choose costumes that are comfortable and not overly frightening. Let your child have a say in picking their costume to ensure it aligns with their sensory preferences.
5. Less Is Best:
Remember, when it comes to costumes, less is often best. Avoid bulky or restrictive outfits that can cause discomfort.
6. Familiar Clothing:
Consider creating costumes from familiar clothing items. This can help your child feel more at ease in their costume.

7. Gradual Costume Familiarization:
Practice wearing the costume for short intervals, starting with just a few minutes and gradually working up to longer periods.
8. Show Costume Varieties:
Show your child pictures of different costumes they may encounter while trick-or-treating. Familiarity can ease anxiety.
9. Avoid Masks:
Most children with SPD don’t like masks. Opt for face paint or makeup instead, which can be less restrictive. Costumes that don’t need a mask, face paint, or makeup may be the best option for some children.
10. Walk the Route:
Before Halloween night, walk the trick-or-treat route a few times with your child to make it familiar and less intimidating.
11. The Joy of Giving:
Remind your child that Halloween isn’t just about receiving treats. Encourage them to be the one who hands out candies to neighbors, which can be a rewarding experience.
12. Early Trick-or-Treating:
Consider going trick-or-treating earlier in the evening, before it gets dark and potentially spookier.
13. Bring a Friend:
Having a friend along can provide extra support and companionship for your child.

14. Respect Their Limits:
If your child becomes tired or no longer wants to participate, don’t push them to continue. Respect their limits and end the evening.
15. Avoid Crowds:
Try to avoid crowded areas and houses while trick-or-treating to reduce sensory overload.
16. Sensory Gear:
Bring noise reduction headphones and sunglasses if your child is sensitive to loud noises or bright lights.
17. Maintain Routine:
Stick to your child’s regular bedtime routine to provide a sense of stability on Halloween night.
18. Sensory Diet:
Complete a sensory diet before and after trick-or-treating, incorporating activities like brushing, joint compressions, heavy work, swinging, or trampolining.
19. Fine Motor Skills:
Have your child attempt to open candy wrappers themselves, which can help improve fine motor skills.

20. It’s Okay Not to Go Out:
Lastly, remember that if your child doesn’t want to go out for Halloween, that’s perfectly okay. Their comfort and well-being should always come first.
Halloween can be a magical time for children, and with these sensory Halloween tips and ideas, you can help your child with SPD enjoy the festivities while minimizing stress and sensory challenges. By being understanding, patient, and supportive, you can create a Halloween experience tailored to your child’s unique needs and preferences.
If you child has been diagnosed with Limb Girdle Muscular Dystrophy and you are interested in learning more about how Schreiber’s Pediatric Therapies can help your child visit: http://www.schreiberpediatric.org/therapy-services/
As a nationally recognized pediatric facility, the Schreiber Center for Pediatric Development provides family-centered education and therapy programs for infants, children and adolescents with disabilities, developmental delays, and acquired injuries. Our goal-oriented approach maximizes each child’s ability to function independently within the community.
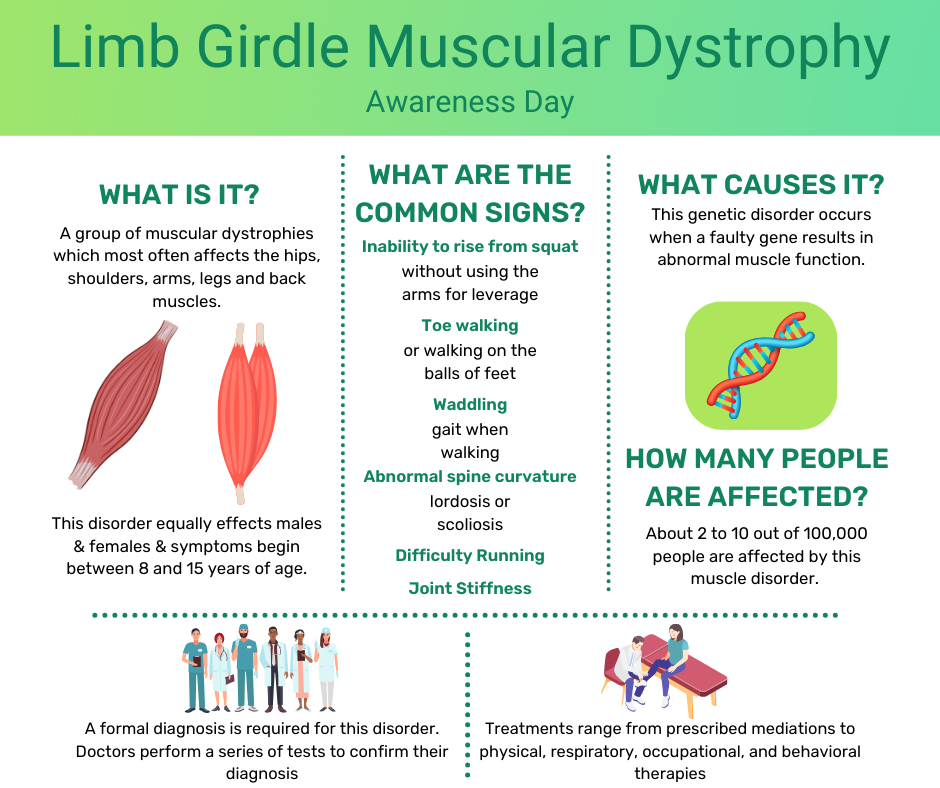
Limb Girdle Muscular Dystrophy
September 29, 2023What is Limb Girdle Muscular Dystrophy?
Limb Girdle Muscular Dystrophy is a group of muscular dystrophies which can be inherited in various ways. It equally effects males and females and symptoms begin between 8 and 15 years of age. About 2 to 10 out of 100,000 people are affected by this muscle disorder which leads to muscle weakness and muscle wasting of varying severity. Most commonly the shoulder and pelvis muscles are affected and as it progresses the hips, shoulders, arms, legs, and back muscles all weaken. The symptoms are known to progress slowly and while there is no cure the life expectancy of an individual with this diagnosis is generally within a normal range since the heart and breathing muscles are not affected.
How do I know if my child has Limb Girdle Muscular Dystrophy?
The signs and symptoms of people with Limb Girdle Muscular Dystrophy can vary widely. Even among individuals within the same family there is a good chance that the signs and symptoms will not be the same. Since symptoms can begin at any age, it’s important to keep an eye out for these common signs throughout your child’s life:
- Inability to rise from a squatting position without using the arms for leverage
- Toe walking or walking on the balls of their feet
- A waddling gait when walking
- Difficulty running
- Joint stiffness
- Abnormal spine curvature (lordosis/scoliosis)
Because these signs and symptoms are common in other muscular dystrophies, it is critical to see a medical doctor and receive a formal diagnosis so that proper treatment can be obtained. The formal diagnosis is based on symptoms, symptom severity, age at which the symptoms began, and family medical history. Doctors will perform a series of tests including: electrodiagnostic tests, laboratory tests, muscle biopsies, imaging studies, electrocardiograms, and genetic testing to confirm their diagnosis.
What Causes Limb Girdle Muscular Dystrophy?
Limb Girdle Muscular Dystrophy is a neuromuscular genetic disorder that occurs when a faulty gene results in abnormal muscle function. Many genes have been identified as contributing to this disorder so while it can be passed from parent to child, the child also could be the first in the family to have muscular dystrophy.
What are the complications of Limb Girdle Muscular Dystrophy?
While it is rare for Limb Girdle Muscular Dystrophy to affect the heart, lungs, digestive system, or other body systems outside of the muscles, it is possible. Any time the heart or lungs are affected by muscular disorders there is a chance that life expectancy will be negatively affected.
What is the treatment of Limb Girdle Muscular Dystrophy?
While there is no cure for Limb Girdle Muscular Dystrophy there are treatments for it. Treatments range from medications that are prescribed by medical professionals to help relieve symptoms relating to Limb Girdle Muscular Dystrophy to physical, respiratory, occupational, and behavioral therapies to help reduce the process of muscle weakness and wasting. Treatment is individualized for each patient and designed to enhance quality of life.
If you child has been diagnosed with Limb Girdle Muscular Dystrophy and you are interested in learning more about how Schreiber’s Pediatric Therapies can help your child visit: http://www.schreiberpediatric.org/therapy-services/
As a nationally recognized pediatric facility, the Schreiber Center for Pediatric Development provides family-centered education and therapy programs for infants, children and adolescents with disabilities, developmental delays, and acquired injuries. Our goal-oriented approach maximizes each child’s ability to function independently within the community.
Anxiety in Kids
September 27, 2023What is Anxiety?
Anxiety is a NORMAL worry or uneasy feeling that causes kids to feel nervous and afraid. It can generate real and uncomfortable physical responses. Anxiety is often triggered by new situations which makes it very common in children. For some children, anxiety affects their behavior and thoughts daily, which can interfere with their home life, school, and their social well-being. For these children, professional help is often the best answer.
Use these tips to help you spot anxiety in your child and help them to learn skills to cope with their anxiety now and in the future.
How Anxiety Feels to Kids
Anxiety can be a confusing and scary feeling for kids, especially if they have never experienced these emotions and physiological effects before and don’t have a name for the way they are feeling. Even once a child knows that they have anxiety and the signs and symptoms they may experience when they become anxious, they may feel embarrassed or ashamed. The physical and psychological symptoms of anxiety can present in a variety of different ways in your child. Look for these common signs.

How Anxiety Shows Up in Kids
If your child is experiencing anxiety, they may begin to act differently. For some kids this may mean that they are acting out and becoming more difficult and defiant, but for other children it might mean that they begin to withdraw from social situations or even their families. It is important to remember that when it comes to anxiety in kids it is not a one size fits all situation. You know your child’s normal behavior better than anyone else, and the best person to determine if their behavior has suddenly or drastically changed. These are a few common signs that are associated with anxiety in kids.

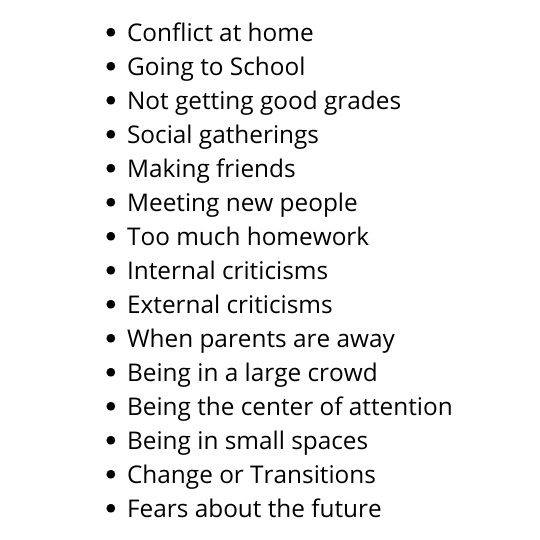
Common Anxiety Triggers for Kids
Since anxiety is often triggered by new situations your child may experience a bout of anxiety occasionally, when something in their life feels different or beyond their control. There are several common triggers for anxiety in kids which range from social factors, or pressure to perform well, to fear of change or the future, and even conflict or change at home. Your child may be experiencing anxiety due to a variety of different things. Below are just a few examples of common anxiety triggers for kids.
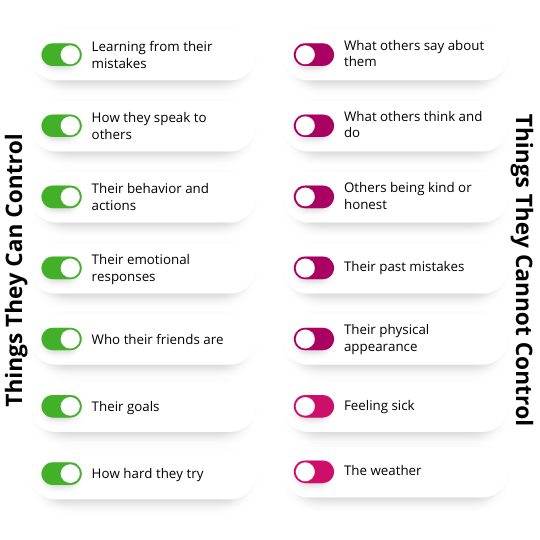
Teach Your Child What They Can & Cannot Control
It can be very helpful to remind your child which things they are feeling anxious about are within their control, and which are not. You may find that much of what your child is anxious about are things they can’t control. So it’s important to teach them the difference between what they can and cannot control, so that they have a better understanding of their own anxieties. It can be helpful for kids with anxiety to have a list that they can refer to that explains these different behaviors. You can use the list below as a starting point and tailor it to your child’s specific anxiety triggers for a helpful guide they can refer to as often as they may need.
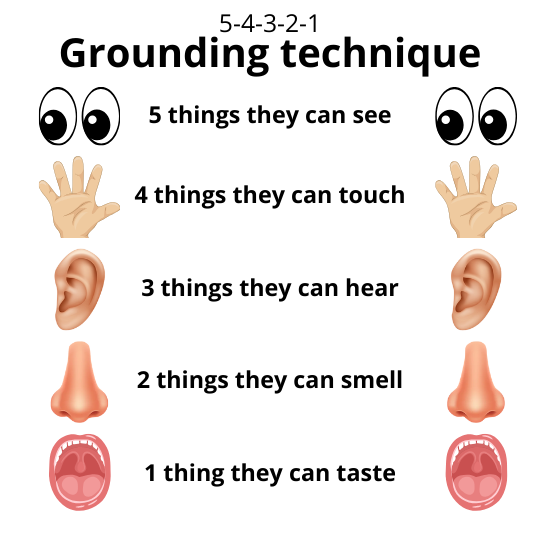
Grounding Techniques for Kids
The 5-4-3-2-1 Grounding technique is helpful both for adults and kids with anxiety as it helps connect the anxious party with the present by exploring the five senses and their immediate surroundings. This technique is especially helpful if the cause of their anxiety is something that already happened or may happen in the future. If the child is currently in the midst of their anxiety trigger the grounding technique may be a bit difficult for them to accomplish, but is still worth an attempt as long as it can be practiced safely. When your child is feeling anxious encourage them to complete the following grounding exercise and see if it helps bring them back to a point of relative calmness. The convenience of being able to perform this technique in almost any location is just one of the many reasons it is so beneficial to learn and remember.
While all children are likely to experience some anxiety in their life on occasion, it is important to recognize if your child’s anxiety has become severe enough to impact their daily lives. If this is the case seeing a pediatric behavioral health therapist may be in your child’s best interest as they can provide more individualistic approaches to help mitigate the causes and symptoms that your child is experiencing. They will also be able to help you and your child understand where the anxiety is coming from and tips, tricks, and tools to help reduce the anxiety your child feels.
If you are interested in learning more about how Schreiber’s Pediatric Behavioral Health Services can help your child visit http://www.schreiberpediatric.org/behavioral-health/
As a nationally recognized pediatric facility, the Schreiber Center for Pediatric Development provides family-centered education and therapy programs for infants, children and adolescents with disabilities, developmental delays, and acquired injuries. Our goal-oriented approach maximizes each child’s ability to function independently within the community.
Sam Leon-Durkee: Young man with a plan
April 19, 2022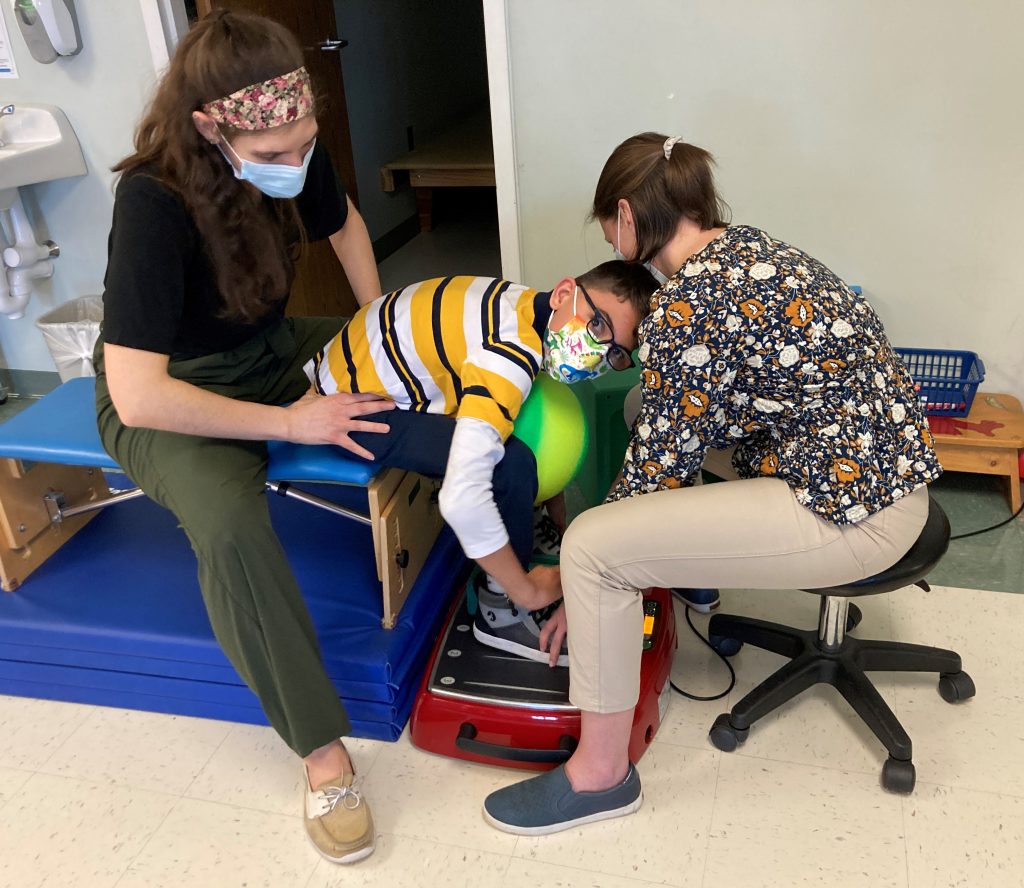
Sam Leon-Durkee started a recent physical therapy session working on a piece of equipment called a Galieleo vibration plate. He sat down on a bench, put his feet on the plate and, with the help of his physical therapist, Rachel Saufley, worked on standing up.
Sam was diagnosed with cerebral palsy at 18 months. He’s 12 now, and does a lot of work to increase his flexibility and mobility. The vibration plate helps reduce the muscle spasticity, or tightness, associated with CP so he can have a more effective therapy session.
Schreiber acquired the vibration plate in December thanks to a grant from the Gamber Foundation. Rachel said she uses it with Sam to help stretch his hamstrings. Sam put it a little differently.

“It’s something new to torture the kids,” he said. “And by torture I mean help.”
He said it like he says a lot of things: with a mischievious smile.
His cerebral palsy makes it hard for him to walk or hold a pencil to write his name. But it has done nothing to hinder his social development.
He’s a talker, a natural storyteller with a vivid imagination and a quick sense of humor. His mom Casey Trone said Sam wants to work at Marvel Comics in New York City.
“I think he’s going to single-handedly write the next Marvel movie,” she said.
That’s the plan right now. For that to happen, there’s still a lot of work to do. Given how far he’s come, though, nobody would bet against it.
Sam was born prematurely in August 2009 and spent five months in the neonatal intensive care unit at Hershey Medical Center. Casey said she started Early Intervention services with Schreiber as soon as she received the diagnosis.
The EI services continued until he was 3. He had a muscle-lengthening surgery at age 4, which helped him make a lot of progress. A year or so later, he returned to Schreiber to resume physical therapy. Around the same time, he started school, first enrolling in Head Start when he was 4 and then starting kindergarten the next year.
“I was a little reluctant,” said Casey, who lives in the Penn Manor School District. “I would have liked to have a little more time for him to develop physically. But he did really well in kindergarten. He’s had an aide with him every year, so the support has been really good.”

He has continued to do well in school, including his middle school years at Manor Middle School.
“He has shocked me,” Casey said. “I remember when I first got the diagnosis of CP, I had no idea what was going to happen. There are so many different forms of the disease. I went so far as to have weight-loss surgery because I didn’t know whether I was going to be able to take care of him. But he’s doing very well.”
A lot of that she attributes to their experience at Schreiber.
“It’s helped me to understand what is possible and what to do and how to take the next step with him,” she said, her voice cracking and a tear rolling down her face. “My life now is to get him to be the best he can be.”
The physical challenges haven’t been the only ones for Casey, Sam and Sam’s twin sister Isabelle. The twins’ father, Henry Leon-Rivera, passed away in 2016. Two years later, Casey brought Mike Trone into their lives.
“They were just about to turn 8,” Mike said. “When we met the first time, we went out for ice cream. We talked a lot about the ‘Cars’ movies. He’s a smaller guy, and he was even smaller then. But he can talk. He knows what he’s talking about. And he has comedic timing. He’s full of life.”
Now it was Mike’s turn to wrestle with his emotions, and he reached over to grasp Casey’s hand.
“I’ve learned so much from him,” he said finally. “I didn’t know anything about CP when Casey and I met. I guess I had a picture in my mind. And he was nothing like that. Resilience is how he approaches day-to-day life. He’s definitely changed my outlook on the world.”
And now the three-person family is four: Casey and Mike married in 2021. She’s financial coordinator with the Library System of Lancaster County. He’s a Realtor with Keller Williams Keystone. Together, they are rebuilding life as a family. And coming to Schreiber to help Sam become his best self, to fulfill his plans of telling the next stories in the Marvel universe.
“I work really hard every day to give Sam the best life I can,” she said. “And I know he meets me halfway to give his best. We all do what we gotta do, and we’ll get there.”

Ellery McIndoe learns to soar at Schreiber
March 29, 2022
Ellery McIndoe has had challenges most people can’t imagine. She also has lots of personality, a big, bright smile and a ton of can-do spirit. In the scheme of things, the challenges don’t seem to be holding her back from being a happy, active, smart 7-year-old little girl.
For her mom Alison, though, getting to this point hasn’t been the easiest journey.
Ellery was born in China, and she spent the first five years living in the orphanage system that China maintains to care for children the government considers to have severe special needs.
Alison, a single parent, had wanted to adopt a young child from China, and she spent several months looking at the profiles of different children with special needs.
“It was a little scary initially,” Alison said. “I passed her by the first few times. You don’t necessarily know the extent of their situation. It could be a heart condition. It could be blindness. I knew very little about her condition.”
She finally learned that Ellery had been diagnosed with arthrogryposis, a rare condition that developed in utero. The condition causes contractures, where one or more joints become permanently fixed in a bent or straightened position, and muscle weakness. Alison knew Ellery had some surgeries in China but not much else about her care.
She adopted Ellery in November 2019. First, she had to help Ellery adjust to her new situation. Five years old, living in a new country with a new language and a new family — it was overwhelming.
“She was very timid and very frightened the first few weeks,” Alison said. “I could literally not be out of her sight at all. She came to work with me, even meetings with clients, and she would just sit there and pretend to take notes, like I did. Or she would make pretend phone calls. She likes to do whatever Mama does.”
Then Alison went to work finding the medical care Ellery needed, starting with surgeries at Nemours Children’s Hospital in Wilmington, Del. In the summer of 2020, doctors operated on her right elbow, wrist and thumb, with the goal of giving her more flexibility in the affected joints and improving her fine motor skills so she would better able to do daily tasks like feeding herself.
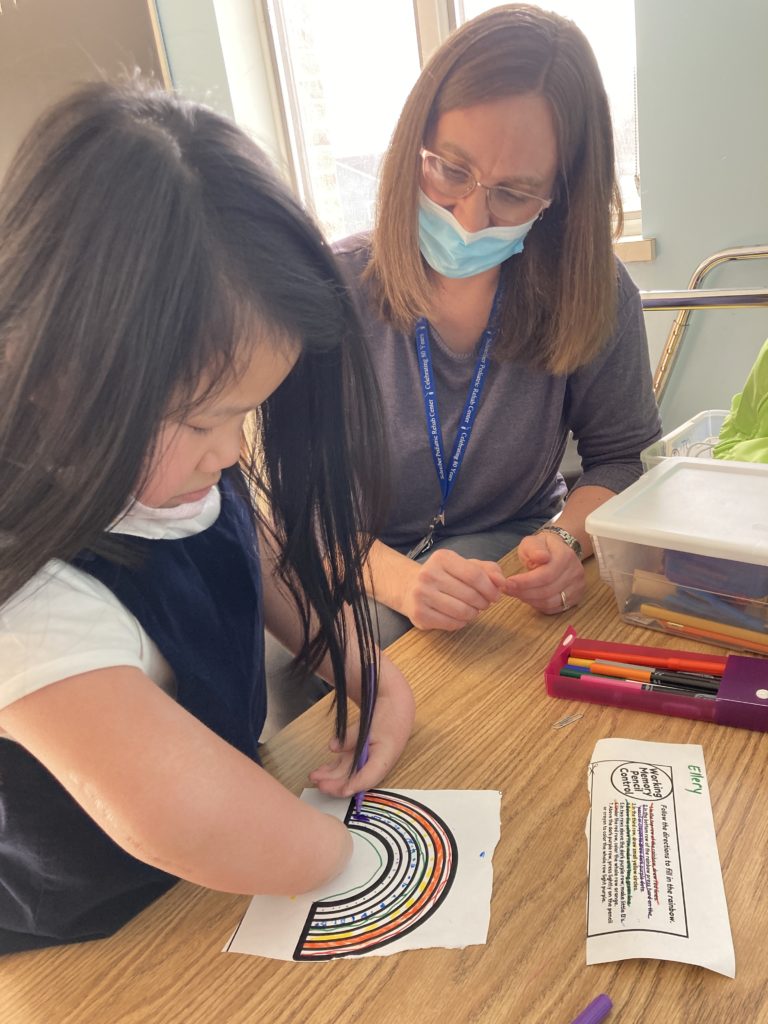
They started coming to Schreiber for services about a year ago. Ellery receives occupational therapy with Amy Mostellar and physical therapy with Christen DeSarro.
“In OT, it’s really a struggle to figure out ways to help her care for herself,” Alison said. “She has fingers, but they don’t move a whole lot. She’s learned to adapt. She can do a lot with her toes: She can color, and she can almost tie her shoes. She loves to swim.
“Just the fact that she sees she can do these things gives her so much confidence. … She just runs with it. She beams.”
Ellery’s newfound confidence shows up in little ways. Like when she smiles and laughs and squeals, “Push me higher,” on the swing in OT.
When she first started at Schreiber, she had trouble grasping her hands together to hold on while she swung. Now? No problem. Those little fingers are stronger.
Or the way she can maintain her balance in PT.
“When she started, she fell all the time,” Alison said. “I worried about her. I thought I might have to get her a helmet, because when she falls, she can’t really catch herself with her arms. Now, she rarely falls. Her balance is so much better. She can walk up the steps now by herself.”
Alison paused.
“I’m still close by though,” she added, with a smile.
She described the progress as slow and steady.
“You almost don’t realize it’s happening. But then you see her on the swing and you think: ‘She couldn’t do that before.'”
The shy, quiet 5-year-old has given way to a confident, bubbly 7-year-old, a foodie (she loves anything spicy) who enjoys sewing (with her feet!) and play dates with friends.
And her experience at Schreiber has played an important part of that evolution.
“(Schreiber) is a wonderful place, and we’re so thankful this is here. This is a joyful place, and Ellery fits right in.”
Carter Peiffer: Back from the brink
March 17, 2022
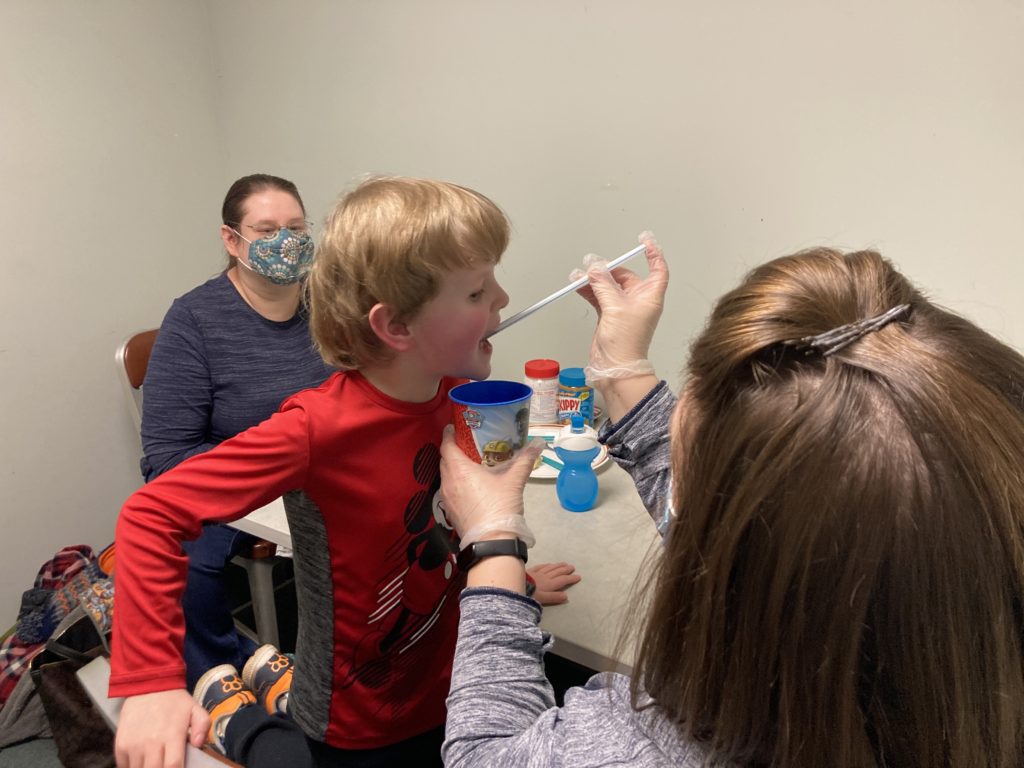
For Carter Peiffer, an occupational therapy session with Sarah Terry will usually involve food. And making a mess with food.
The mess is by design. A puddle of PediaSure on the table is fair game for Carter to write his name in, drive a toy car through or give a sip to Elmo. He might pull a straw from a cup filled with the nutrition drink and sniff (good) or take a tiny taste (better) from the end of the straw.
It’s all about making food fun for Carter, giving him positive experiences. He and food have had a rough two years. Through a series of life events, Carter went from a happy, active 2 year-old who would eat lots of different foods to a 4 year-old who would only eat strawberry banana yogurt — and it had to be Gerber’s. The lack of variety and nutrition in his diet over time left him with a severe vitamin C deficiency and a case of what used to be called scurvy. That caused his bones and muscles to weaken, to the point where his bones became brittle and he couldn’t walk or even stand without help.

Let’s go back to the beginning. When he was 2, his mother Desiree said she noticed Carter was a little delayed in speech. But he was otherwise active and healthy. Then he gradually began to cut out some foods, starting when Carter’s brother was born. Around the same time, his grandmother was in the hospital for an extended period following heart surgery.
These new stresses in his life caused him to become even more picky with his eating, to the point where all he would eat was the yogurt.
In March a year ago, Carter was running around playing when he tripped and fell. He ended up breaking the growth plate in his left knee, which required a knee immobilizer. A month later, he fell again — still wearing the immobilizer on his right knee — and broke the growth plate in his other knee.
After another round of medical visits, doctors at Children’s Hospital of Philadelphia in May found multiple tiny fractures in his bones and sent him to CHOP’s emergency department for an immediate, intensive examination.
Their conclusion: Carter’s increasingly limited diet for more than a year had caused a dangerous vitamin C deficiency that had weakened his bones and left him susceptible to fractures. His overall medical state was as fragile as his little brittle bones.
He spent nine days at CHOP in May receiving treatment and starting inpatient therapy. Later that month, after he was sent home, Desiree called Jen Bachman, our social services director, to arrange starting services at Schreiber.
In early June, Carter had his first physical therapy visit. After not being able to put any weight on his legs because of his knee injuries, step one in his recovery was relearning how to walk. He did aquatic therapy in our therapy pool with Megan Campbell Roland, and PT in the gym with Laurie Panther.
Desiree said Laurie noticed some sensory issues and suggested Carter be evaluated for occupational therapy. In September, doctors diagnosed him with autism and sensory processing disorder, and he started working with Sarah for OT. The work there has focused on helping him expand the variety of foods he ate.
“Carter, what did you eat today?”
Sarah asked the question at the start of a recent therapy session.
“Some peanut butter bread, and I ate some hot dog!”
“You did not,” Mom said. She smiled and gave him a what-are-you-talking-about look. “You had some yogurt.”
“Yogurt,” Carter repeated back, and then swirled some PediaSure around the table with his fingers.
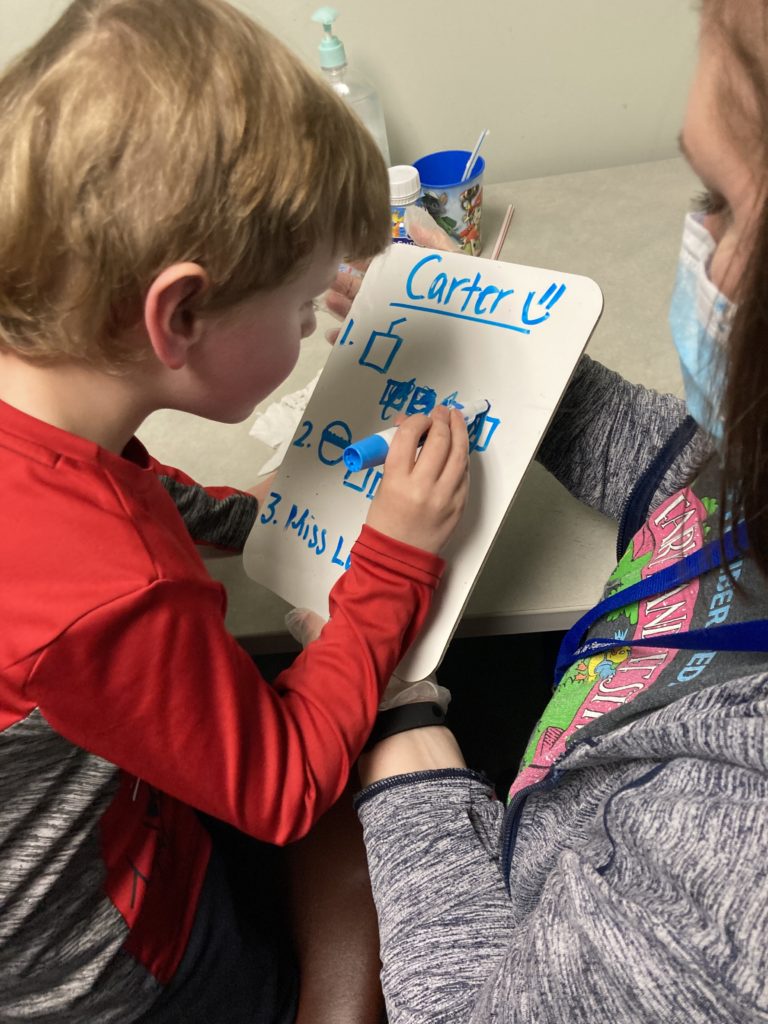
Sarah had a dry erase board next to her with Carter’s eating goals for the session written in blue marker. When Carter accomplished one of his tasks for the session, Sarah had him fill in the box next to that task on the white board.
The work with Sarah on eating is paying off. Desiree said Carter weighed 29 pounds when he arrived at CHOP a year ago and 32 pounds when he left. Today, his weight consistently ranges between 42 and 45 pounds.
“Sarah got him to eat peanut butter and marshmallow (sandwiches),” she said. “He started eating chips. He tried an animal cracker and a pretzel. He seems to like the crunchy stuff.”
It’s a constant process, sometimes painfully slow, sometimes with setbacks.
“When he gets derailed, when he gets sick, he shuts down (and stops eating),” she said. “I’ve had to stay up all night with him to give him water, because getting dehydrated would mean we’d have to go to the ER.”
The progress is obvious, and not just with his eating.
“He’s able to walk and run and is almost back to where he was before all this started,” Desiree said. “He plays on the playground. He goes up and down steps. He’s able to express himself more now.”
Later, she talked with a lot of emotion about what she has seen bringing him to every appointment for the past nine months.
“To see his progress has been amazing. I know (coming to Schreiber) will all end at some point, but everybody has been so amazing. They are like family here, and Carter loves being here.”
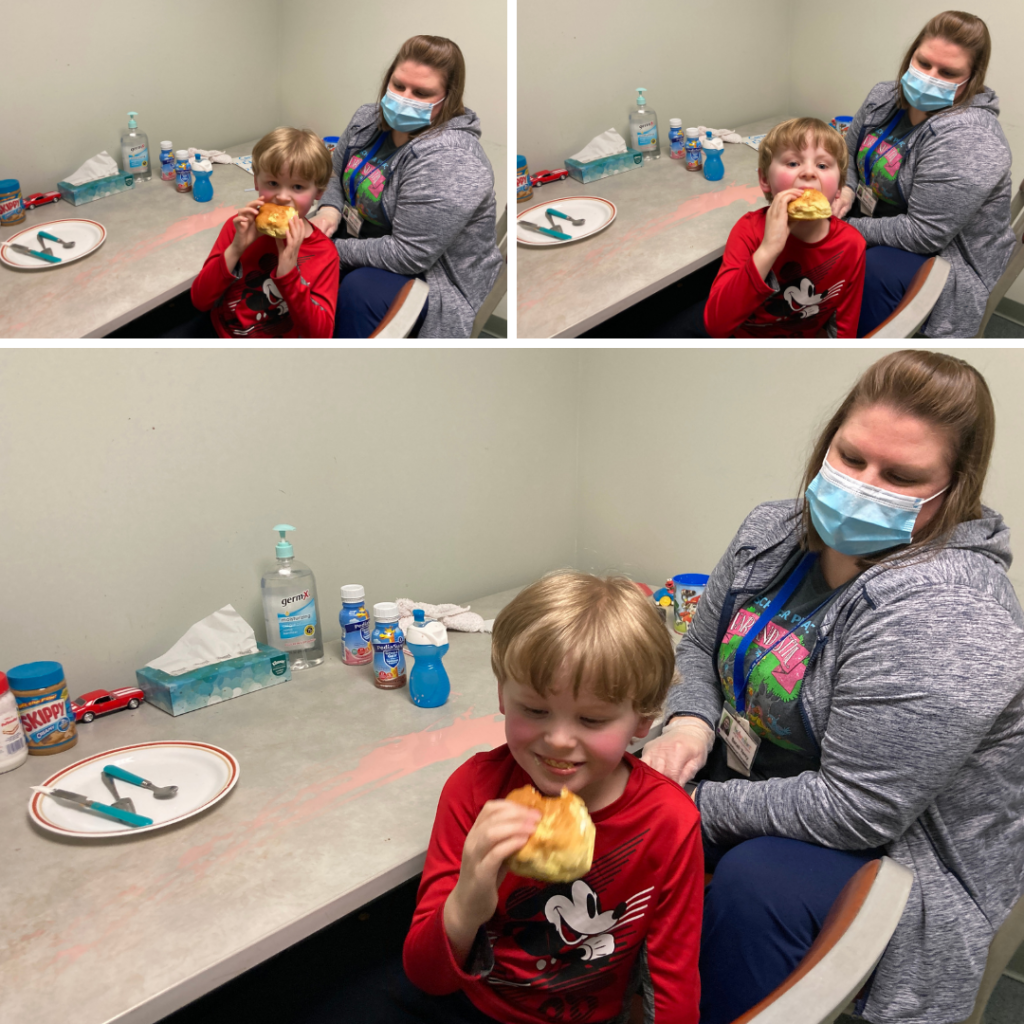
After taking two tentative tastes of a strawberry nutrition drink, Carter finishes the session with a reward: a bite of his peanut butter sandwich.
For the Kiss family, dedication mixed with gratitude
March 4, 2022
The complications for Colton Kiss started the moment he was born. His mom, Tara Kiss, said doctors used vacuum extraction to help with delivery.
The procedure “caused four intracranial brain hemorrhages,” Tara wrote in an email, “as well as a blood clot on his cerebellum, which is the part of the brain that controls movement, balance and speech.”
Colton was quickly transferred from Lancaster to Children’s Hospital of Philadelphia, widely known as CHOP, where he spent the next two weeks in the neonatal intensive care unit (NICU). Tara, living in York at the time, stayed with her mother, Cathy Kiss. Cathy lives in Manor Township, and Tara drove back and forth to Philadelphia every day for those two weeks to be with Colton.
When Colton was 4 months old, a follow-up MRI showed the blood clot and hemorrhages were gone, but the clot left behind an area of damage on the cerebellum.

“We learned from his neurologist that we were looking at a long road of obstacles as that part of the brain is so important to everyday life — walking, talking, motor skills…,” Tara wrote.
CHOP referred them to Early Intervention and outpatient pediatric therapy. After doing some research and talking with friends, Tara knew she wanted to start services with Schreiber. Cathy’s best friend’s father, Joe Finger, had volunteered here with a group of other residents from St. Anne’s Retirement Community. Cathy also knew Michele DeBord, sister of Schreiber President James DeBord.
“Hearing about (Joe’s) experience and knowing Michele was so passionate about Schreiber, we were really comfortable (starting at Schreiber),” Cathy said.
Colton was born in March of 2020. Tara moved to Lancaster in December of that year to start services at Schreiber.
“We were immediately welcome by the Schreiber staff who are now pretty much our family,” Tara wrote. “Lisa (Moore, at the front desk) took us in under her wing and connected me to Jen Bachman to get Colton evaluated and started right away. We have been working with Miss Christen (DeSarro) for PT, Miss Kim (Martin) for OT and Miss Cassie (Glick) for speech. When we started, Colton was unable to sit unassisted, unable to feed himself solid food, unable to say any words at all.”
That was where Colton was in early 2021. Today? He still receives all three therapies, and he’s enrolled in Schreiber’s Circle of Friends Academy child care program, in the Toddler Room.
“Whether children are born healthy or born with already known obstacles, every child deserves a chance to be helped, and Schreiber gives every child a fair chance at a normal life.”
Tara Kiss, Colton’s mother
“It has not even been a year yet,” Tara wrote, “and he is now able to sit, stand alone and take his own steps on flat surfaces. He can feed himself any type of food he desires. He is working on his words and attempting new words almost daily. We are only in the beginning of this journey, but because of the dedication from our Schreiber family, Colton has a chance to live his life as normal as possible.”
Which is why Cathy reached out just about a year ago at this time offering to help with our first Cup O’ Cards fundraiser. The idea for Cup O’ Cards was simple: We bought a bunch of gift cards from local businesses, stuffed them into some sponsored coffee cups, then raffled off the cups.
“I heard about it from Michele, I looked at your website, and I decided to jump right in” by donating a card-filled coffee cup, she said.
Cathy, who runs her own home-based accounting business, CLK Accounting and Payroll Inc., reached out to a number of clients and asked them to donate money to buy gift cards or to donate cards from their business. We quickly added her CLK Accounting mug to the other cups, and it turned out to be popular with raffle ticket buyers.
She was happy to participate in the second Cup O’ Cards raffle, which starts March 28, and she plans to do two cups this year, including a Mystery Cup filled with a collection of surprise gift cards.
“I’ve already raised more than $600 in cash, which I’ll use to buy the gift cards,” Cathy said, “and collected two donated items for the Mystery Cup.”
Last year, with Cathy’s help, Cup O’ Cards raised about $27,000. This year, with her help again, we hope to raise even more. And that would be make a proud grandmother pretty happy.

“That’s my boy,” she said. “And I see what Schreiber does for kids with my own eyes. (Colton) didn’t sit up until he was maybe 10 or 11 months old. He’s very delayed. To see his progress with the therapists is what I love about Schreiber.”
Tara said it this way in her email:
“… Whether children are born healthy or born with already known obstacles, every child deserves a chance to be helped, and Schreiber gives every child a fair chance at a normal life. That is something I will always support. We are forever grateful for Schreiber and the care my son receives. From his teachers at Circle of Friends Academy down to all of his therapists, thank you all for loving my son!”
Winter Olympics come to Schreiber
February 2, 2022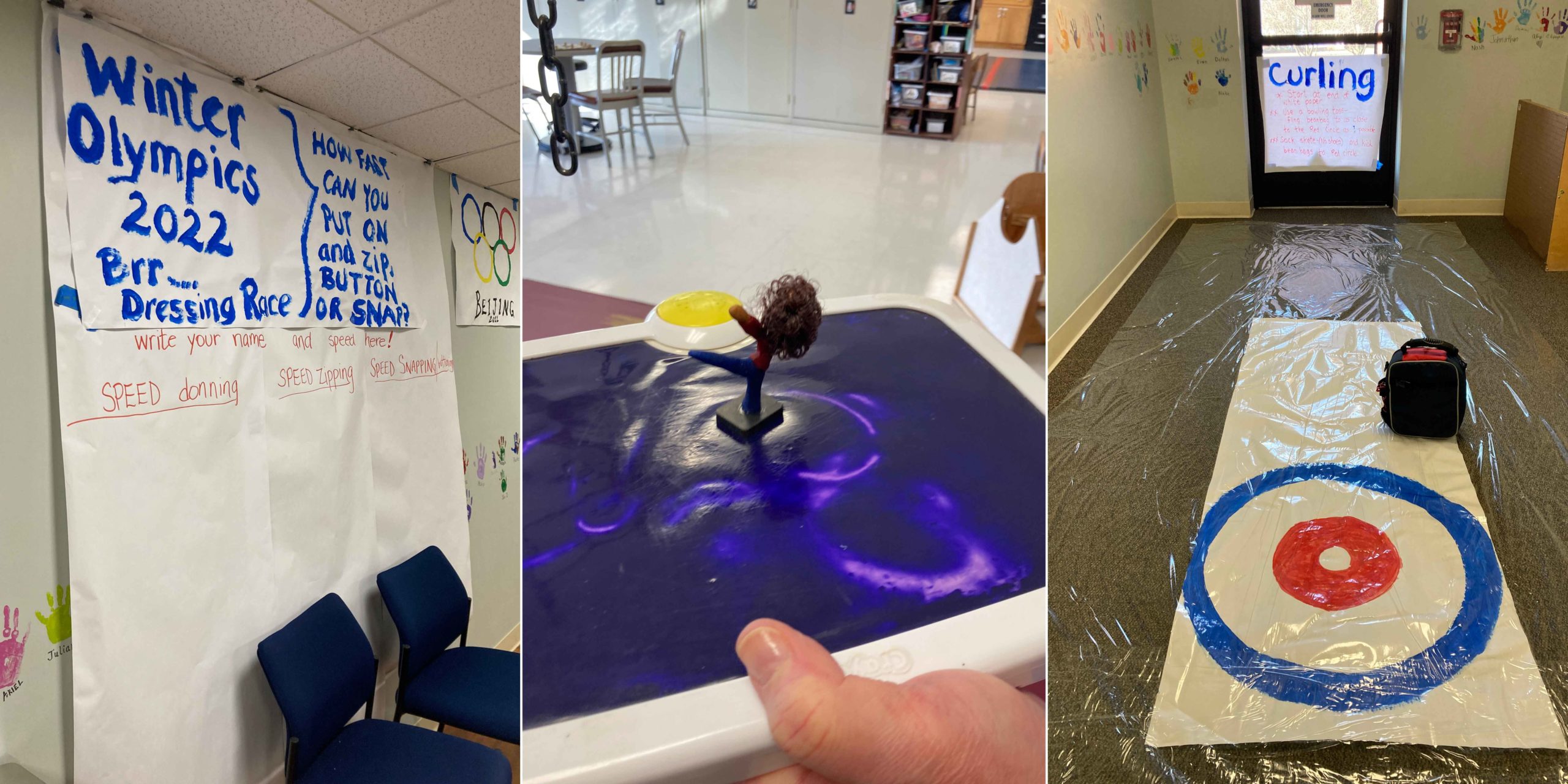
The Winter Olympics begin Feb. 4 in China. On the other side of the world, right here in Lancaster County, we have our own version of the Games at Schreiber.
Over the next few weeks, while you’re here at the center, you might notice the unusual Olympic-inspired decorations. There’s the Speed Dressing arena outside of Occupational Therapy, where competitors will be testing themselves on Speed Donning, Speed Zipping and Speed Snapping. Next to that is the Curling hallway. There will be several areas for Olympic hockey, including table top Knock Hockey and air hockey along with a hockey net (or at least a drawing of one taped to a wall – video below) to shoot pucks at, and hand-held games for to compete in figure skating.
And the main event will almost certainly be in the Activities of Daily Living Room, home to the luge and Bobsled track.
These are mostly the work of OT Bernie Hershey, who regularly finds some of the more outside-the-box creative ways to add fun to therapy sessions. All of the activities incorporate therapy work into the game playing. And therapists in OT, physical therapy and speech-language pathology are using the games.
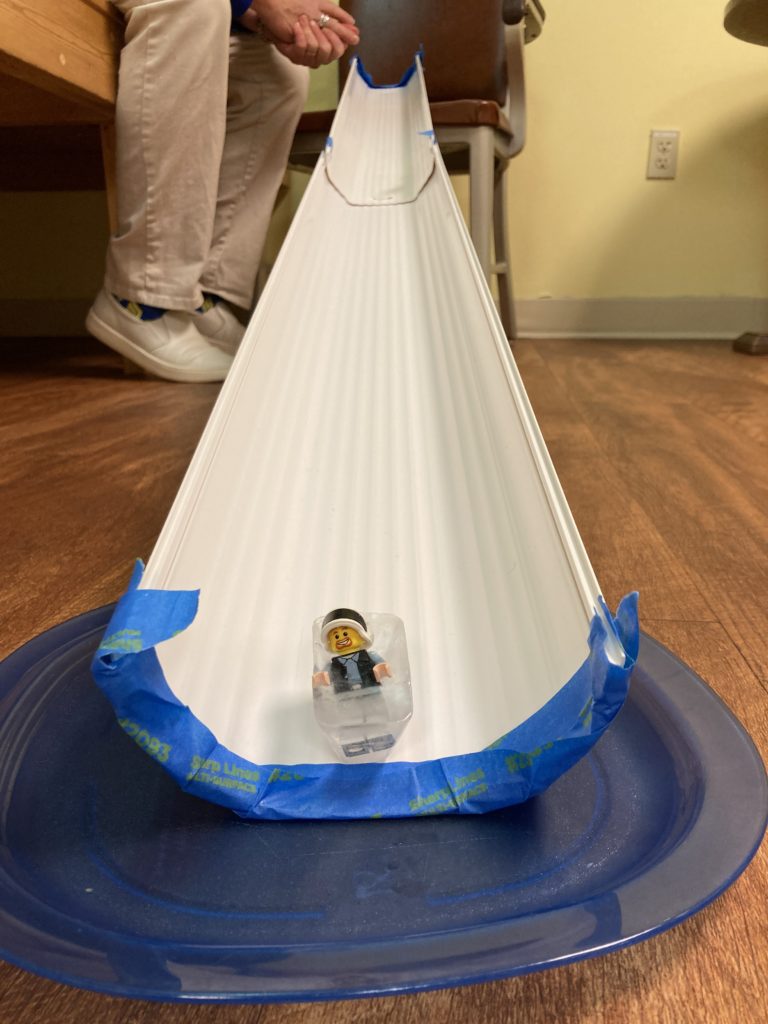
Occupational Therapist Bernie Hershey has organized a series of Olympic-style events for kids to include in their therapy for the next few weeks during the Winter Olympics. Here, a bobsledder finishes a run.
“Anything that breaks up the normal routine and adds a little fun helps,” Bernie said. “I like looking for ways to include what’s going on in the world with our therapy.”
Speed Dressing helps kiddos work on how quickly they are able to dress themselves, often a goal for many of the kids we see. Curling helps with gross motor skills. Knock Hockey and air hockey works on eye-hand coordination. The luge and bobsled races and some of the figure skating helps with pinching and grasping.
Schreiber mom: From advocate for others to advocate for son
December 17, 2021
Amanda Katchur is a psychologist who has been an advocate for services that support children for a number of years. Now, she’s learning to advocate for her own child, and that’s a completely different experience.
It’s one thing to know professionally the impact that Schreiber’s services and Lancaster County’s Early Intervention program have on families. It’s another thing to see it personally.
Her daughter Bethany was diagnosed as an infant with torticollis, a condition in infants that causes a baby’s head to tilt constantly to one side. Thanks to the work of Schreiber therapists, Bethany’s torticollis is gone and she runs, jumps and dances just like any 6-year-old little girl, Amanda said.
Bethany’s little brother Leo, 3 years old, has an autism diagnosis, was born with mild hearing loss and also had some torticollis as an infant. The three issues combined have left him behind in several areas of development. When it was time for Leo to receive services through Early Intervention, at 6 months old, Amanda had no hesitation.
“I knew we wanted to come back (to Schreiber) because we had such a positive experience with Bethany,” Amanda said.
Leo has been in good hands his therapy services started. Catherine Donahue was his Schreiber’s Early Intervention specialist for home visits. Dorlas Riley was his speech-language pathologist. Denisha Roberts worked with him in physical therapy. And Bernie Hershey has been his occupational therapist.
I like to think that we’ve been fortunate to have, like, the dream team…, with all the experience they have with his issues.
AMANDA KATCHUR
“They were all really great,” Amanda said. “I like to think that we’ve been fortunate to have, like, the dream team to be quite honest with you, with all the experience they have with his issues.”
COVID has, at times, made the therapy more challenging, like when the family had to switch to telehealth services for a time. At those moments, she could see the lengths the Schreiber team would go to for a child.
When telehealth sessions switched back to in-person visits, the change and the lack of consistency caused some challenges for Leo, as it does for many kids on the autism spectrum.
“Bernie showed up at one point at our house in costume as Jessie from “Toy Story” to try to re-engage after telehealth with Leo a little bit,” Amanda said. “They just really always made an attempt (to find what) he was interested in and get into his world, which I appreciated so much.”
During a recent therapy session at Schreiber, Leo worked with Marli Hess, an intern in Occupational Therapy, and Maddy Sova, a speech-language pathologist. They were trying to help him become more comfortable with a different kind of food – in this case, a chicken nugget – and to improve his language skills by using a smart tablet to respond to questions.
“We are working on communication in whatever way Leo feels most comfortable,” Amanda said. “Today, you saw him working on some eating, because eating has been a struggle for us, too. So he’s been working on increasing his tolerance for different foods and different textures and things like that. But communication has been, I would say, the biggest one.”
Mom was impressed with the way Leo greeted a visitor to the session, smiling and waving. “He probably wouldn’t have done that six months ago,” she said.
EI services do make a difference

Mandy Kolb Lyons is a coordinator in Lancaster County’s Early Intervention services program. She sent this email to agencies that provide Early Intervention services after a recent presentation to the agencies by Amanda Katchur. Amanda presented at the PA Statewide Interagency Coordinating Council (SICC) meeting to share her family’s story and how Early Intervention supported them.
Here’s an excerpt from Mandy’s email:
“Amanda shared numerous examples of how you helped to coach, support, empower and guide her and her family. Amanda beamed as she shared the journey that her son and family had with Early Intervention and mentioned a few times how Early Intervention supported her entire family, including Leo’s big sister! Not only did Leo grow and progress throughout services, his entire family did. We can only hope that every family that participates in Early Intervention can walk away feeling similarly to how Amanda and her family did after participating in our services.”